Who needs a heart transplant?
A heart transplant is a last-resort treatment for people who have end-stage heart failure. That means your heart has permanent damage or weakness that keeps it from pumping enough blood to your body.
This kind of heart failure can happen for a wide variety of reasons. Most people who need a heart transplant have one of the following conditions:
- Cardiomyopathy. This refers to any disease that damages your heart muscle (cardio = heart, myo- = muscle, pathy = disease). Causes include infections and genetic diseases. Sometimes, the cause is unclear (idiopathic) even after extensive testing.
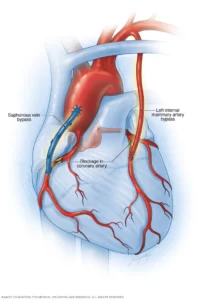
- Coronary artery disease. Blockages in the arteries in your heart can lead to heart attacksthat cause irreversible damage to your heart.
- Congenital heart disease. Congenital heart disease is a defect in the heart’s structure that you’re born with. Some forms of congenital heart disease can lead to end-stage heart failure, which may require a heart transplant.
- Valvular heart disease. These are conditions that involve damage to your heart valves.
Heart transplants are possible for children and adults up to age 70 and in some circumstances up to age 75.
What happens before a heart transplant?
The following steps happen before your heart transplant surgery:
- Referral to a transplant program.
- Transplant evaluation.
- Addition to the waiting list.
- Bridge treatment.
- You receive ongoing medical treatment while awaiting transplantation.
- You may need support with a mechanical device while awaiting transplantation.
These steps are described in greater detail below.
Referral to a transplant program
To begin the process, your healthcare provider must refer you to a heart transplant program. Then you can schedule your evaluation.
Transplant evaluation
There aren’t enough available heart donors to provide a heart to everyone who needs one. So, the evaluation ensures that you have the best chance to benefit from one long-term.
Your transplant evaluation includes several parts.
Medical evaluation
Your healthcare provider checks your overall health by running several different tests. Some, but not all, of the possible tests are listed below.
Lab testing includes blood and urine tests that examine your:
- Blood composition. Your provider checks the levels of red blood cells, platelets and other components in your blood. They also analyze your blood chemistry to look for signs of other conditions that might affect your ability to have a heart transplant.
- Immune system. Your provider uses the findings from an immune system analysis to predict how well your immune system can tolerate a donor organ.
- Kidney function. A urinalysis shows how well your kidneys are working.
- Use of alcohol, tobacco and drugs. Testing for alcohol, tobacco and drugs is an important part of your preparation. You must avoid alcohol, tobacco products (including vaping) and recreational drugs (including marijuana) for an extended time before your transplant.
Imaging tests you may need include:
- X-rays.
- Computed tomography (CT) scans.
- Magnetic resonance imaging (MRI).
- Echocardiogram.
Diagnostic tests check the function of your heart, respiratory and circulatory systems. These may include:
- Electrocardiogram (ECG or EKG).
- Exercise stress testing.
- Pulmonary (lung) function testing.
- Heart catheterization.
- Holter monitor.
Testing for specific diseases is also possible, especially the following:
- Tuberculosis.
- HIV.
- Hepatitis B.
- Hepatitis C.
- Toxoplasmosis.
- Herpes simplex virus.
- Varicella-zoster virus (the virus that causes chickenpox and shingles).
Transplant recipients need to be up-to-date on vaccines before transplantation. An infectious disease specialist helps with this process.
Psychological and neurological evaluation
Part of the selection process includes psychological and neurological testing and evaluation. That’s because maintaining a healthy heart transplant is stressful and at times challenging. People who receive a transplant also face an increased risk of depression. Neurological tests check for issues that might cause you additional problems.
Dental evaluation
Your oral health, especially the condition of your teeth, can play a big role in your heart health. It’s common for oral infections from cavities to spread to your heart and cause damage there.
Social and financial evaluation
Heart transplant is a difficult, intensive process. People with the best chance of success also have a good support system around them, including family and friends. The transplant team will talk with you about your situation and learn what resources you might need to get through the process.
Bridge treatment
Bridge treatments are therapies, medications or other types of care that help you while you wait for a transplant. These therapies help you have fewer and milder symptoms.
Potential bridge treatments include:
- Medications. These medications affect your heart function in different ways, such as making your heart beat faster or pump harder.
- Mechanical support. Certain types of devices can help your heart pump. An example is an intra-aortic balloon pump. A doctor inserts this pump into a major blood vessel and threads it up to your heart until it’s just outside your heart’s aortic valve. The pump then inflates and deflates a small balloon in time with your heart. This makes it easier for your heart to pump.
- Left ventricular assist device. Your heart may be so weak that it pumps an inadequate amount of blood to your body. This can lead to organ damage. In this case, your team may recommend a left ventricular assist device to keep you safe while awaiting transplantation.
What happens during a heart transplant?
A heart transplant is a complicated surgery. Your care team will perform the following steps.
- Give you general anesthesia. A heart transplant always involves general anesthesia, which puts you into a deep sleep.
- Connect you to a ventilator. While you’re asleep, your provider inserts a tube down your throat, attaching the end of the tube outside your body to a machine called a ventilator. The ventilator keeps you breathing even though you’re under anesthesia.
- Give you blood thinners. Your provider adds a blood thinner like heparin to your blood. This reduces the risk of blood clots as your blood flows through the heart-lung bypass machine.
- Connect you to a heart-lung bypass machine. This is also called a cardiopulmonary bypass machine. This device takes over the work of your heart and lungs during your surgery. It adds oxygen to your blood and removes carbon dioxide. It also keeps your blood circulating to all your other organs and tissues.
- Remove your heart. To make room for the donor heart, your surgeon removes your heart. This procedure involves clamping off the blood vessels that connect to your heart and disconnecting your heart from them.
- Implant the donor heart. Your surgeon attaches the donor heart to your major blood vessels and starts to warm and restart your new heart. Your new heart may need help to start beating. If so, your care team may need to use an electrical pacing device. This device works like a pacemaker but doesn’t involve permanent implantation.
What happens after a heart transplant?
After your heart transplant, you can expect the following:
- Hospital recovery. You’ll recover in the hospital for one to three weeks, depending on your situation. You’ll spend the first part of your recovery in the intensive care unit (ICU). In the ICU, healthcare providers will monitor you around the clock. They’ll check your vital signs and also watch for any signs that your body is rejecting your new heart.
- Plan of care. Before you leave the hospital, your provider will give you a plan of care that you should follow while recovering at home. Make sure you understand the plan, and ask as many questions as needed.
- Cardiac rehab. Your provider will tell you how to join a cardiac rehabilitation program. This is a prescribed, monitored program that helps you improve your strength, endurance and heart function.
When you’re back home, it’s important to closely follow your plan of care. Your plan will include instructions for:
- Medications you need to take.
- What to eat and drink, and what to avoid.
- Exercise and physical activities that are safe vs. unsafe.
- Recognizing signs of infection or organ rejection.
It’s also essential to learn what’s normal during recovery, and what signals a problem. One example is knowing what your resting heart rate should be.
After your heart transplant, your resting heart rate usually stays at the high end of normal or slightly higher (90 to 110 beats per minute). This is because the donor heart doesn’t automatically connect with your body’s nervous system, which controls your heart rate. Talk with your provider about the resting heart rate you can expect and how it might change in the future.
heart transplant surgery recovery time
Your healthcare provider is the best person to tell you when you can return to your usual activities. It depends on how your recovery is going and your overall health.
You likely won’t be able to drive for at least six to eight weeks after your surgery. You also shouldn’t lift anything heavier than 10 pounds for at least six weeks. Your provider will give you specific instructions that you should closely follow.
Immune system suppression
After your surgery, your provider will start you on medications that suppress your immune system. These immunosuppressants are essential medications for transplant recipients.
That’s because your immune system’s normal reaction to a foreign object (like a donor heart) is to treat it like an infection or other harmful invader and attack it. The immunosuppressant medications protect your new heart from attack by your own immune system. You’ll need to take these medications for the rest of your life
Cost of Heart Transplant Surgery in India
Heart Transplant cost in India for Indian Patients is between USD30000 to USD40000. Cost for International patients is between USD 45000 to USD 55000.
Patient has to stay in the hospital for 20 days and outside the hospital for 30 days. The total cost of the treatment depends on the diagnosis and facilities opted by the patient.
Success Rate
The overall survival rate after Heart Transplant is more than 85% after one year and about 69% after five years for adults.
It takes around three to six months for complete healing after a Heart Transplant. However, the age and general health of an individual also depend on the recovery period.
Cardiac Surgeons in India
Cardiac surgeons in India are known for their expertise in identifying and providing medical intervention for complex and critical cardiac conditions. In the year 2022, they have performed over 70,044 cardiovascular surgery procedures, showcasing their proficiency and dedication to improving heart health. Moreover, they specialise in the latest technologies, such as minimally invasive cardiac surgery and Da Vinci robotic-assisted surgery.
The specialised skills and knowledge they have earned through years of experience make them pioneers in the medical field.